Question: 
There is so much information on the internet regarding celiac disease and the gluten-free diet but it’s hard to distinguish fact from fiction. Shelley, please help me demystify and make sense of all this information!
Answer:
Here are 10 Facts about celiac disease and the gluten-free diet, including links and resources that I have put together to help people learn more about the disease and its treatment:
1. Celiac disease affects 1:100 people.
Celiac disease is one of the most common inherited disorders, with an estimated prevalence rate of 1:100. It can develop at any age, even in the senior years. It is twice as common as Crohn’s, ulcerative colitis and cystic fibrosis combined. Click here for more information about celiac disease
2. Diagnosis of celiac disease is often delayed.
Delay in diagnosis is common. Studies in the US and Canada have found that it can take over 10 years before an accurate diagnosis is made. Many individuals are frequently misdiagnosed with other conditions such as irritable bowel syndrome, ulcers, allergies, chronic fatigue syndrome and fibromyalgia prior to getting the correct diagnosis.
3. Anemia is a common symptom of celiac disease.
Anemia is a condition that results from a deficiency in the size or number of red blood cells or the amount of hemoglobin in these cells. There are many causes of anemia; however, the most common is due to iron, folate or vitamin B12 deficiency. In celiac disease, damage to the intestinal villi in the area where iron and folate are absorbed, frequently results in a deficiency of these nutrients. Once a diagnosis of celiac disease is confirmed and the gluten-free diet is initiated, the villi begin to heal which allows for the absorption of nutrients. Response to the gluten-free diet varies from one individual to another and may take on average from 2-18 months until the nutritional deficiencies are corrected and symptoms resolve. For more information see Anemia and Celiac Disease – Causes and Treatment.
4. Dermatitis Herpetiformis is related to celiac disease.
Dermatitis Herpetiformis (DH) is another form of celiac disease. This chronic skin condition is characterized by an intense burning, itchy and blistering rash. The rash is symmetrically distributed and commonly found on the elbows, knees and the buttocks, but can also occur on the back of the neck, upper back, scalp and hairline. Initially, groups of small blisters are formed that soon erupt into small erosions. Most people with DH will also have varying degrees of small intestinal villous atrophy although many will have no bowel complaints. A small percentage may present with bloating, abdominal pain and diarrhea, especially if the bowel involvement is severe, and some individuals may show evidence of malabsorption and malnutrition. Treatment for DH is a strict gluten-free diet for life. For some individuals, Dapsone, a drug from the “sulphone family,” may be prescribed to reduce the itching. Response to the medication can be dramatic (usually 48-72 hours). However, Dapsone has no effect on the ongoing immune response or intestinal atrophy. See this article to find out more about DH.
5. Some people with newly diagnosed celiac disease also have lactose intolerance.
In celiac disease the small intestinal villi (tiny finger-like projections) become inflamed and flattened (known as villous atrophy) due to the reaction to gluten. The tips of the villi also contain enzymes such as lactase which is responsible for the digestion of lactose- a natural sugar found in milk and milk products. In some individuals with newly diagnosed celiac disease, especially those with major villous atrophy, the level of lactase is significantly reduced. This temporary lactose intolerance causes undigested lactose to pass through the intestinal tract, drawing fluid with it. It is then fermented by bacteria in the large intestine producing short-chain fatty acids and gases. Symptoms of lactose intolerance may include abdominal cramping, bloating, gas, nausea, headache and diarrhea. These symptoms can occur 15-30 minutes or as long as several hours after consuming foods with lactose.
The good news is that this temporary lactose intolerance often improves on the gluten-free diet alone. However, some people may also need to restrict or reduce lactose until the villi are completely healed and the lactase enzyme levels are restored to normal. This may take weeks to months depending on individual response. It should be noted that most individuals with lactose intolerance can digest small amounts of lactose. Here are some tips to manage lactose intolerance.
6. A strict gluten-free diet is the only treatment for celiac disease.
The only treatment for CD is a strict gluten-free diet for life. All forms of wheat, rye and barley must strictly be avoided, including spelt, kamut, einkorn, emmer, faro, durum, couscous, semolina, bulgur and triticale. Barley malt, barley malt extract, barley malt flavor, brewer’s yeast, malt vinegar, as well as barley-based ale, beer and lager must also be avoided. Here is a more detailed list of foods allowed, to avoid and to question.
7. Pure uncontaminated oats are allowed on a gluten-free diet.
The protein in oats was originally thought to trigger the same toxic reaction as wheat and other gluten-containing grains. Research in Europe and the US over the past 15 years has revealed that consumption of moderate amounts of oats is safe for the majority of children and adults with celiac disease. Most of these studies used pure, uncontaminated oats, but it should be noted that a very small number of individuals with celiac disease may not tolerate pure oats. The mechanism causing this intolerance has yet to be established. Before adding pure, uncontaminated oats to your diet, talk to your doctor and dietitian. Most authorities recommend that individuals with celiac disease be well established on the gluten-free diet, the celiac antibodies have returned to normal and symptoms resolved. For more information about the safety of oats see this link.
8. Many foods are gluten-free.
A wide variety of foods that are naturally gluten-free include plain meat, poultry, fish, eggs, legumes, nuts, seeds, milk, yogurt, cheese, fruits, vegetables, as well as many gluten-free flours, cereals and starches that can be substituted for wheat, barley and rye. Distilled alcoholic beverages, wine and gluten-free beer made from buckwheat, millet, rice or sorghum are also allowed.
Amaranth, buckwheat, corn, flax, Indian ricegrass (Montina), legume flours (bean, chickpea/garbanzo bean, pea, lentil), mesquite, millet, nut flours, potato flour, potato starch, quinoa, rice, sago, sorghum, soy, tapioca and teff are gluten-free options.
A growing number of gluten-free specialty products from companies in the USA, Canada and Europe are available in health food and grocery stores, as well as mail order companies. Examples include ready-to-eat baked products (e.g., breads, buns, bagels, muffins, cakes, cookies, pies, pizza crusts), baking mixes and specialty flours, hot and cold cereals, crackers, snack foods, entrees, pastas (corn, legumes, quinoa and rice), bread crumbs, coating mixes, gravy mixes, soups, sauces, communion wafers, ice cream cones, snack bars and gluten-free beers.
Check out Gluten-Free Diet: A Comprehensive Resource Guide for a detailed listing of foods allowed, over 3100 gluten-free specialty products from more than 270 companies, meal plans, recipes, nutrition guidelines and many other resources.
9. Consulting a registered dietitian with expertise in celiac disease is good advice.
A dietitian will do a nutritional assessment, teach you about celiac disease and the gluten-free diet, and give you practical information to help you successfully manage the gluten-free diet.
10. There are excellent celiac groups in North America.
Join a celiac group for additional support and encouragement. Here are links to celiac organizations in the US and Canada.
Ask Shelley Case is a feature of BeFreeForMe.com. It is published the second Tuesday of each month. Shelley Case, RD is a Consulting Dietitian, Speaker and Author of Gluten-Free Diet: A Comprehensive Resource Guide. Visit Shelley and get more gluten-free tips & info at: GlutenFreeDiet.ca
 Question:
Question: Question: My child was diagnosed with celiac disease a year ago. Over the summer we found it easy to eat gluten-free with all the fresh fruits, vegetables, outdoor picnics & barbeques. Now that fall is here we are struggling to get into the swing of things, not to mention having to deal with Halloween. Any ideas?
Question: My child was diagnosed with celiac disease a year ago. Over the summer we found it easy to eat gluten-free with all the fresh fruits, vegetables, outdoor picnics & barbeques. Now that fall is here we are struggling to get into the swing of things, not to mention having to deal with Halloween. Any ideas? Answer:
Answer:  Council recommend at least 3 to 5 servings of whole grains per day. The average adult who consumes 2000 calories/day (the amount on the nutrition label), should eat 6 grain servings a day – making at least half of them whole grains. To make things simple and find smart choices, look for the yellow
Council recommend at least 3 to 5 servings of whole grains per day. The average adult who consumes 2000 calories/day (the amount on the nutrition label), should eat 6 grain servings a day – making at least half of them whole grains. To make things simple and find smart choices, look for the yellow 
 : Check out the photograph below that Shelley took of one of these beautiful sunsets!)
: Check out the photograph below that Shelley took of one of these beautiful sunsets!)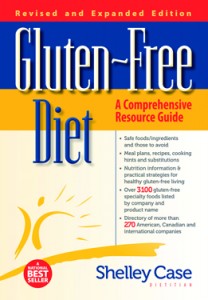
 Question:
Question: 
 Question: Since getting diagnosed with celiac disease, I feel like I’ve been buying and eating “anything and everything” as long as it is gluten-free! Now that it’s the New Year, I need some tips for getting back on track and take some control over my diet, especially since I have gained unwanted extra pounds. Do you have ideas for healthy gluten-free eating?
Question: Since getting diagnosed with celiac disease, I feel like I’ve been buying and eating “anything and everything” as long as it is gluten-free! Now that it’s the New Year, I need some tips for getting back on track and take some control over my diet, especially since I have gained unwanted extra pounds. Do you have ideas for healthy gluten-free eating?  snacks with these healthy foods. Check out
snacks with these healthy foods. Check out 
 Question: I am on a gluten-free diet and need help with meal planning. Do you have any suggestions on making meal time a bit more exciting by adding more variety? P.S. – Healthy & nutritious ideas are a plus too!
Question: I am on a gluten-free diet and need help with meal planning. Do you have any suggestions on making meal time a bit more exciting by adding more variety? P.S. – Healthy & nutritious ideas are a plus too!